Start Here
Welcome to my CRPS Journey

What is Complex Regional Pain Syndrome (CRPS)?
Complex Regional Pain Syndrome (CRPS) used to be known as “Reflex Sympathetic Dystrophy.” RareDiseases.org describes CRPS as: “a disorder in which pain, occurring spontaneously or from a sensory stimulus, is disproportionately far more painful than it should be.” They go on to describe that sensations may include increased sensitivity, burning feelings, or even numbness. Swelling; edema (fluid retention); temperature changes both hot and cold; weakness; decreased range of motion; as well as skin, nail, and hair changes are also common symptoms of CRPS.
Type I CRPS follows an injury, in my case a broken leg bone (tibia). Type II CRPS is rarer and there is documented nerve damage in those cases. Researchers and medical professionals are unclear as to what, exactly, causes CRPS.  Risk factors include:
Risk factors include:
- wearing a cast after an injury.
- changes in the sympathetic nervous system that is in charge of “fight or flight” reflexes.
- abnormally increased inflammation.
It is theorized that genetics may play a part in who is more susceptible to CRPS. Psychological factors like depression and anxiety may worsen CRPS but it is not a cause of the illness. [1]
The Budapest Criteria
Doctors typically use the Budapest criteria for diagnosing CRPS.
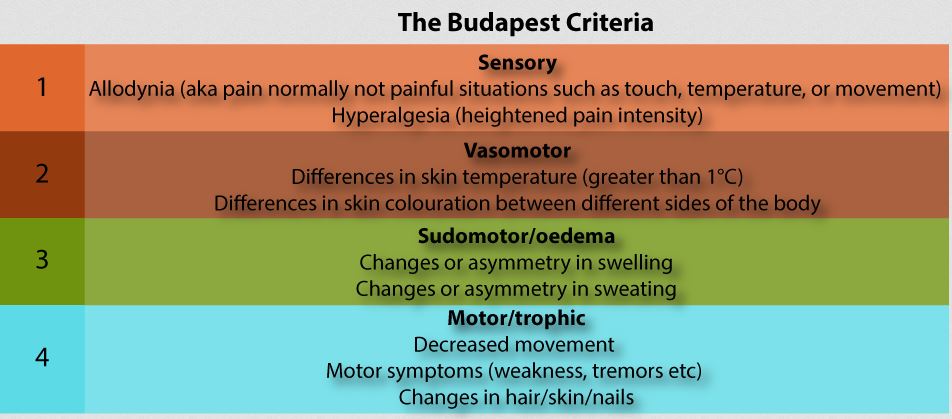
Figure from Speaking of Research.
How CRPS is Treated
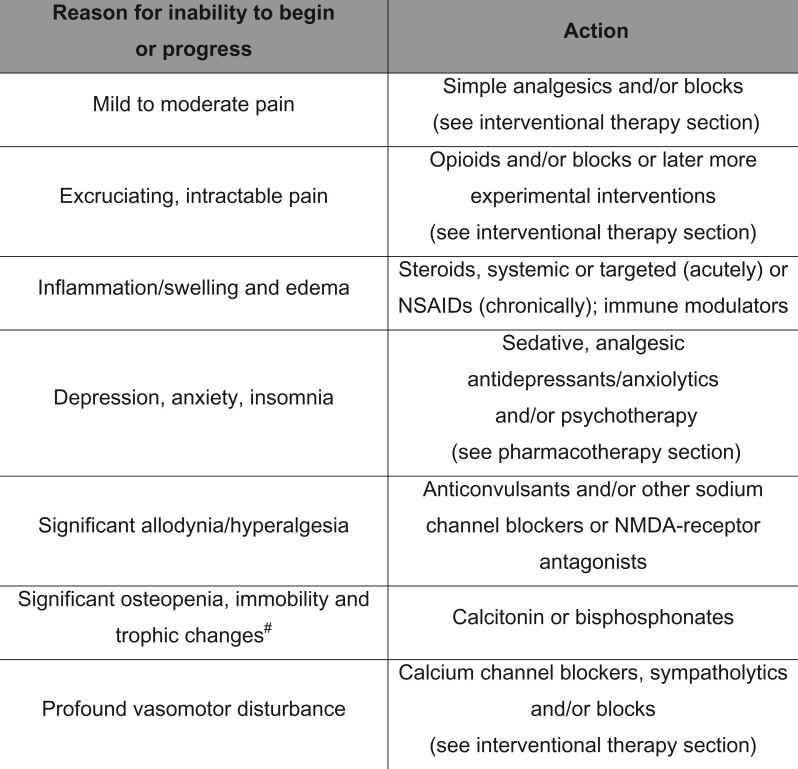
Figure from Complex Regional Pain Syndrome: Practical Diagnostic and Treatment Guidelines, 5th Edition. Harden et al.
My Experience with CRPS

It All Started With a Broken Leg
After I broke my leg in January 2024, I was in a hard cast for 6 weeks. This is typical of a clean break that does not need surgery. After 6 weeks, I felt that the pain was still too great to transfer to a boot but followed my orthopedist’s recommendation and began wearing a boot. I did experience some improvement. When I had my 4 week follow up with the doctor (10 weeks post-break) I still had symptoms like swelling and discoloration of the foot and ankle. My doctor examined my foot and told me that I had CRPS. He called it a “classic case” and even asked if a student could come in to look at it! He acted very casual about it, as though it were common. He said essentially that sometimes the nerves get “turned on” by the injury and don’t turn off. The doctor said that he would refer me to pain management and they would “reboot my nerves with a steroid shot, kind of like how you reboot a computer.” I wasn’t thrilled to have a new diagnosis but as I told my friends and family “it sounds scary but it really isn’t a big deal! I just have to have a shot.” Then, I read up on CRPS on the internet. The reality of life with CRPS for most people was NOT as simple as my doctor made it sound!
As I read about people’s real life experiences, I started to get scared. My pain was in the 2-4 range on a scale of 1-10 but there were people out there living in constant, excruciating pain. People talked about having no symptoms for three years and then all of a sudden, one day waking up in excruciating pain. I started to get concerned, reading about treatments not working or even making things worse. What was this illness I had been so casually diagnosed with?
My Symptoms
- Swelling in the foot, toes, and ankle that did not improve over time.
- Pitting edema (fluid in the foot and ankle that would not immediately bounce back when pressed.)
- “Pins and needles” feeling on the bottom of my foot at times but not all the time.
- Extreme discoloration whenever my foot was not elevated. Change in color happened almost immediately when not elevated.
- The discoloration progressed up my leg to my calf as I began to put weight on the foot.
- Skin on my foot looked uneven and “mottled” darker in some places even when elevated.
- Random numbness. Sometimes one toe would go numb, then another would. Sometimes just the bottom of my foot would be numb.
- Random pain. I would also have pain in just one toe, then another.
- Referred pain. I would have pain that seemed to spread around my ankle so that it hurt on the opposite side from where it was broken.
- “Popcorn” feeling in my foot and leg. Random popping feeling that was similar to the popcorn feeling but also different.
- Feeling of warmth to the foot and leg when touched.

Next Steps
Disclaimer
I am not a medical professional and I am not an expert on CRPS. I am not providing medical advice here, only sharing my personal experiences. This should not be substituted for medical advice from your own doctor. Everyone’s experience is different.